by Buck Institute
May 18, 2022 . Press Release
Buck Scientist Uncovers Clues to Aging in Mitochondria
Many age-related diseases share a common feature: the mitochondria of cells begin to malfunction. While the cause is not known, Buck Institute scientists have discovered a new mechanism of how mitochondria start to go wrong, which opens new doors for researchers to explore how to begin to fix the problem.
 “Now that we have this different hypothesis of why mitochondrial dysfunction happens during aging and age-related diseases, we open a completely different way to think about, measure, mitigate and reverse that process,” said Buck Fellow Chuankai (Kai) Zhou, PhD, who is the senior author of a study published in the March 2 issue of eLife, a leading journal on biomedical research established by the Howard Hughes Medical Institute, Max Planck Society, and Welcome Trust.
“Now that we have this different hypothesis of why mitochondrial dysfunction happens during aging and age-related diseases, we open a completely different way to think about, measure, mitigate and reverse that process,” said Buck Fellow Chuankai (Kai) Zhou, PhD, who is the senior author of a study published in the March 2 issue of eLife, a leading journal on biomedical research established by the Howard Hughes Medical Institute, Max Planck Society, and Welcome Trust.
Mitochondria are commonly referred to as the “powerhouse” of the cell, as the bean-shaped structures provide the units of energy that every cell needs to function. They are involved in many critical processes, including immune response, inflammation, and metabolism.
Dysfunction of the mitochondria is implicated in most chronic diseases, said Zhou, including neurodegenerative disorders, cardiovascular diseases, cancer, diabetes, and obesity. A growing body of evidence indicates that this dysfunction contributes to aging in general.
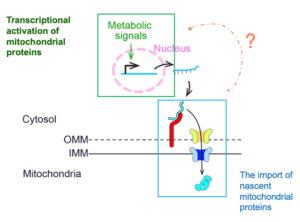 Zhou’s team wanted to explore the contributions of “mitochondrial biogenesis” to the dysfunction of mitochondria during aging. Mitochondrial biogenesis is the cellular process that produces new mitochondria. It determines both the quality and quantity of mitochondria in cells, both of which decline during normal aging. In the past couple decades, scientists already described two major steps of mitochondrial biogenesis: the transcriptional activation of mitochondrial protein in the cellular nucleus in response to nutrient/metabolic signals and the import of these newly synthesized mitochondrial proteins from cytosol into mitochondria. However, it was unclear how these two steps of mitochondrial biogenesis coordinate with each other to streamline the synthesis and import of mitochondria proteins. Zhou’s team found that a conserved receptor molecule on the surface of mitochondria called Tom70 might be responsible for coordinating these two steps by regulating the transcriptional activity of mitochondrial proteins inside nucleus.
Zhou’s team wanted to explore the contributions of “mitochondrial biogenesis” to the dysfunction of mitochondria during aging. Mitochondrial biogenesis is the cellular process that produces new mitochondria. It determines both the quality and quantity of mitochondria in cells, both of which decline during normal aging. In the past couple decades, scientists already described two major steps of mitochondrial biogenesis: the transcriptional activation of mitochondrial protein in the cellular nucleus in response to nutrient/metabolic signals and the import of these newly synthesized mitochondrial proteins from cytosol into mitochondria. However, it was unclear how these two steps of mitochondrial biogenesis coordinate with each other to streamline the synthesis and import of mitochondria proteins. Zhou’s team found that a conserved receptor molecule on the surface of mitochondria called Tom70 might be responsible for coordinating these two steps by regulating the transcriptional activity of mitochondrial proteins inside nucleus.
Tom70 is previously known to facilitate the import of newly synthesized mitochondrial proteins. However, Zhou noted, the amount of protein created must be fine-tuned to meet the needs and import capacity of the mitochondria but not overshoot production such that excess accumulates within the cell, which damages cells and can kill them.
In the current study, his team used yeast as the model to test whether Tom70 regulates mitochondrial biogenesis by coordinating the intricate balance between the production of proteins destined for the mitochondria and the rate that these proteins can be escorted into the mitochondria. They found that it did. Similar regulatory function of Tom70 is conserved in fruit flies.
The two processes of communication about needs and uptake into the mitochondria had not been previously linked. “Our research finding that the molecule Tom70 is coordinating both aspects bridges two separate fields of study,” said Zhou.
Interestingly, they found that Tom70 declines during aging, which is associated with reduced mitochondrial biogenesis. Similar reductions of Tom70 were observed previously in aged fruit flies and rats. The team went on to show that increasing the level of Tom70 in yeast delayed mitochondrial dysfunction and increased lifespan. This finding ties in with what was known for more than a decade, that increasing Tom70 can protect human cells against some chronic diseases, such as cardiovascular disease, but the mechanistic details were not known about why this occurred. “We discovered a new function for this protein and we provide a mechanism of how Tom70 can do good things to the cell,” said Zhou.
Zhou said he can envision a number of ways in which this understanding can point to new directions in aging research. For example, the Tom70 pathway is linked to the lifespan increases seen with caloric restriction. “Additionally, if our hypothesis proves to be true, it will naturally lead to products, such as supplements or drugs. It just takes time,” he said.
For himself, Zhou said he plans to dive deeper into yeast genetics to uncover the specifics of the mechanism, such as how Tom70 communicates with the nucleus. “That is the beauty of basic research, it really gives you something to explore that did not exist before,” he said. “We are excited about translation, but we are even more excited about something brand new, that no one knew about before.”
Citation: Tom70-based transcriptional regulation of mitochondrial biogenesis and aging
DOI: /10.7554/eLife.75658
Additional Buck collaborators include Qingqing Liu, Catherine E. Chang, Alexandra Wooldredge, and Benjamin Fong, as well as Brian Kennedy, Centre for Healthy Longevity, National University Health System, Singapore, Singapore.
The work was funded by the Glenn Foundation for Medical Research; NIH Office of the Director (DP5OD024598), and National Institute on Aging (R01 AG058742) (R03AG070478)
Science is showing that while chronological aging is inevitable, biological aging is malleable. There's a part of it that you can fight, and we are getting closer and closer to winning that fight.
Eric Verdin, MD, Buck Institute President and CEO